Myths & Facts About Aging
 This article delves into ageist stereotypes dressed-up in the garb of myth that biases perceptions and experiences of being old. The article argues current ”mythmaking” about aging perpetuates that which it intends to dispel: ageism. It considers how traditional myths and folklore explained personal experience, shapes social life, and offers meaning for the unexplainable. The current myths of aging perform these same functions in our culture; however, they are based on half-truths, false knowledge, and stated as ageist stereotypes about that which is known. Recent studies in the cognitive sciences are reviewed to provide insight about the mind’s inherent ability to construct categories, concepts, and stereotypes as it responds to experience. These normal processes need to be better understood, particularly regarding how social stereotypes are constructed. Finally, the article argues that ageist stereotypes when labeled as ”myth” even in the pursuit of the realities of aging, neither educate the public about the opportunities and challenges of aging nor inform social and health practitioners about the aged.
This article delves into ageist stereotypes dressed-up in the garb of myth that biases perceptions and experiences of being old. The article argues current ”mythmaking” about aging perpetuates that which it intends to dispel: ageism. It considers how traditional myths and folklore explained personal experience, shapes social life, and offers meaning for the unexplainable. The current myths of aging perform these same functions in our culture; however, they are based on half-truths, false knowledge, and stated as ageist stereotypes about that which is known. Recent studies in the cognitive sciences are reviewed to provide insight about the mind’s inherent ability to construct categories, concepts, and stereotypes as it responds to experience. These normal processes need to be better understood, particularly regarding how social stereotypes are constructed. Finally, the article argues that ageist stereotypes when labeled as ”myth” even in the pursuit of the realities of aging, neither educate the public about the opportunities and challenges of aging nor inform social and health practitioners about the aged.
Think you know the facts about growing older? Think again.
Take a brief quiz to determine your knowledge on myth versus fact as it relates to aging:
Myths of Aging Quiz – Answer true or false to each statement.
- Polypharmacy (administration of many drugs together) can lead to a change in mental status.
- Aging is a universal phenomenon.
- Older adults may present with atypical symptoms that complicate diagnosis.
- The body’s reaction to changes in medications remains constant with advancing age.
- If the rehabilitation nurse observes a sudden change in mental status in an older adult, medication side effects should be investigated as a likely cause.
- Primary causes of delirium in older adults include medications, dehydration, and infection.
- Dehydration is not common in older adults.
- Older adults experiencing a decline in daily function will show no benefit from early rehabilitation.
- A decline in functional ability for a person residing in a long-term care facility may indicate the onset of a new illness.
- Urinary incontinence is so common in older adults that it is considered a nor- mal part of aging.
Answers: 1. True; 2. True; 3. True; 4. False; 5. True; 6. True; 7. False; 8. False; 9. True; 10. False
In no particular order… what are the common 20 myths that are often associate with Aging
Myth: Dementia is an inevitable part of aging
“Dementia should be seen as a modifiable health condition and, if it occurs, should be followed as a medical condition, not a normal part of aging. In other words, if you or your loved one becomes forgetful, it could be related to medication, nutrition or modifiable medical issues, she said. Don’t assume Alzheimer’s.
Just consider that when doctors examined the brain of a 115-year-old woman who, when she died, was the world’s oldest woman, they found essentially normal brain tissue, with no evidence of Alzheimer’s or other dementia-causing conditions. Testing in the years before she died showed no loss in brain function.
Not only is dementia not inevitable with age, but you actually have some control over whether or not you develop it. “We’re only now starting to understand the linkages between health in your 40s, 50s and 60s and cognitive function later in life. Studies find that many of the same risk factors that contribute to heart disease—high blood pressure, high cholesterol, diabetes and obesity… may also contribute to Alzheimer’s and other dementias.
For instance, studies on the brains of elderly people with and without dementia find significant blood vessel damage in those with hypertension. Such damage shrinks the amount of healthy brain tissue you have in reserve, reducing the amount available if a disease like Alzheimer’s. That’s important, because we’re starting to understand that the more brain function you have to begin with, the more you can afford to lose before your core functions are affected.
Myth: Creaky, Achy Joints are Unavoidable
Not exercising is what makes achy joints inevitable. When Australian researchers at the Monash University Medical School looked at women ages 40 to 67, they found that those who exercised at least once every two weeks for 20 minutes or more had more cartilage in their knees. It suggests that being physically active made them less likely to develop arthritis.
In Fact – You may actually dodge the dementia bullet… Exercise your body and your brain. Physical activity plays a role in reducing the risk of diseases that cause Alzheimer’s. It also builds up that brain reserve. One study found just six months of regular physical activity increased brain volume in 59 healthy but couch-potato individuals ages 60 to 79. Other research finds people who exercised twice a week over an average of 21 years slashed their risk of Alzheimer’s in half.
Then there’s intellectual exercise. It doesn’t matter what kind, just that you break out of your comfort zone. Even writing letters twice a week instead of sending e-mail can have brain-strengthening benefits. That’s because such novel activities stimulate more regions of the brain, increasing blood flow and helping to not only build brain connections, but improve the health of existing tissue.
Myth: If you didn’t exercise in your 30s & 40s, it’s too late to start in your 50s, 60s or 70s
It’s’s never too late! In an oft-cited study, 50 men and women with an average age of 87 worked out with weights for 10 weeks and increased their muscle strength 113 percent. Even more important, they also increased their walking speed, a marker of overall physical health in the elderly.
Myth: Your Bones Become Fragile And Your Posture Bends
Remember, only death is certain when it comes to aging. Osteoporosis is definitely more common in older people, but it’s also very preventable.
A study of females over 100 years of age found that only 56 percent had osteoporosis, and their average age at diagnosis was 87. Not bad, given these women grew up before the benefits of diet and exercise on bone were understood. Thankfully, you know better.
Myth: Old Age Kills Your Libido
Impotence and reduced libido are related to normally preventable medical conditions like high blood pressure, heart disease, diabetes, and depression. The solution is keeping yourself in shape. Something as simple as lifting weights a couple times a week can improve your sex life. Sexual desire might decline a bit as you age, but that doesn’t typically occur until age 75A survey of 3,005 people ages 57 to 85 found the chance of being sexually active depended as much if not more on their health and their partner’s health than on their age. Women who rated their health as “very good” or “excellent” were 79 percent more likely to be sexually active than women who rated their health as “poor” or “fair.” And while fewer people ages 75 to 85 had sex than those 57 to 74, more than half (54 percent) of those who were sexually active had intercourse two or three times a month. emember – Sexually transmitted diseases do not discriminate based on age. If you’re not in a monogamous relationship, you or your partner should use a condom.
Myth: Getting older is depressing so expect to be depressed
No way! “Depression is highly treatable. If older people could just admit to it and get help, they could probably live a much more active and healthy life.” That’s because studies find that older people who are depressed are more likely to develop memory and learning problems, while other research links depression to an increased risk of death from numerous age-related diseases, including Parkinson’s disease, stroke and pneumonia.
Myth: Genes Play The Biggest Role In How You’ll Age
Even if you’re born with the healthiest set of genes, how you live your life determines how they behave over your lifespan. Your genes can be changed by what you eat, how much physical activity you get, and even your exposure to chemicals.
Myth: Women fear aging more so than men
Not so! A survey conducted on behalf of the National Women’s Health Resource Center found that women tend to have a positive outlook on aging and to be inspired by others who also have positive attitudes and who stay active as they grow older. Women surveyed were most likely to view aging as “an adventure and opportunity” and less likely to view it as depressing or a struggle.
Myth: You Lose Your Creativity As You Age
Creativity actually offers huge benefits for older people. A study found that older adults who joined a choir were in better health, used less medication, and had fewer falls after a year than a similar group that didn’t join. The singers also said they were less lonely, had a better outlook on life, and participated in more activities overall than the non-singing group, who actually reduced the number of activities they participated in during the year.
Myth: The pain and disability caused by arthritis is inevitable, as you get older
 While arthritis is more common as you age, thanks to the impact of time on the cushiony cartilage that prevents joints and bone from rubbing against one another, age itself doesn’t cause arthritis. There are steps you can take in your youth to prevent it, such as losing weight, wearing comfortable, supportive shoes (as opposed to three-inch spikes), and taking it easy with joint-debilitating exercise like running and basketball. One study found women who exercised at least once every two weeks for at least 20 minutes were much less likely to develop arthritis of the knee (the most common location for the disease) than women who exercised less.
While arthritis is more common as you age, thanks to the impact of time on the cushiony cartilage that prevents joints and bone from rubbing against one another, age itself doesn’t cause arthritis. There are steps you can take in your youth to prevent it, such as losing weight, wearing comfortable, supportive shoes (as opposed to three-inch spikes), and taking it easy with joint-debilitating exercise like running and basketball. One study found women who exercised at least once every two weeks for at least 20 minutes were much less likely to develop arthritis of the knee (the most common location for the disease) than women who exercised less.
Myth: Your Brain Stops Developing After Age 3
This developmental myth was overturned in the 1990s, and ever since, researchers no longer look at the older brain as a static thing. Instead, studies show your brain continues to send out new connections and to strengthen existing ones throughout your life — as long as you continue to challenge it. It really is your body’s ultimate muscle.
Myth: Your Brain Shrinks With Age
This myth began with studies in 2002 showing that the hippocampus, the part of the brain that controls memory, was significantly smaller in older people than in younger people. This never sounded right to Dr. Lupien, particularly after she conducted groundbreaking research in the late 1990s showing that chronic stress shrinks the hippocampus.
Was it age or stress that was responsible for the shrinking brains of older people? Probably stress. When she examined brain scans of 177 people ages 18 to 85, she found that 25 percent of the 18- to 24-year-olds had hippocampus volumes as small as those of adults ages 60 to 75.
Myth: Seniors Are Always Cranky And Unhappy
When researchers from Heidelberg, Germany, interviewed 40 centenarians, they found that despite significant physical and mental problems, 71 percent said they were happy, and more than half said they were as happy as they’d been at younger ages. Plus, when the researchers compared them to a group of middle-age people, they found that both groups were just as happy. Most important: Nearly 70 percent of the centenarians said they laughed often. What does it all mean? It means there is no universal definition of aging. How you’ll age is entirely up to you – and the time to begin writing that definition is today.
Myth: When you get older, you don’t need as much sleep
You may need as much sleep as when you were younger, but you may have more trouble getting a good night’s sleep. “It is not so much that there is a decline in the number of hours needed, but rather that sleep patterns may change with a tendency to more naps and shorter nighttime periods of deep sleep.
Myth: If you live long enough, you’re going to be senile
The odds are against it. “The probability of senility at age 65 is only about five percent. It rises to about 20 percent by age 85.
The term “senility” is no longer used to describe dementia. Alzheimer’s disease is the most common type of primary progressive dementia. Alzheimer’s is linked to age, Dr. Gorbien says, and older people worried about it should seek an assessment with a geriatrician, neurologist or psychiatrist.
“Early detection of Alzheimer’s disease is so important,” he says. New medications may slow the progression of the disease and help keep people independent.
Myth: Older adults are always alone and lonely
In proportion the number of older people living alone are greater than their younger counterparts, but they are not necessarily lonely. Relationships may grow more intense in old age, Dr. Schaie says. More people live alone as the population ages, Dr. Gorbien says. And Dr. Schaie says gender differences in average life spans leave many more women than men widowed. Widowed men are more likely than women to remarry, Dr. Schaie says, “because of the availability of a larger pool of eligible partners.”
“Most seniors are active,” adds AARP spokesman Tom Otwell. Many have paying jobs, regularly volunteer, garden or help care for grandchildren, for instance.
Myth: Old age means losing all my teeth
If you’re not worried about losing your mind when you’re old, you might fret about losing your teeth. Periodontitis, or late stage gum disease, is the primary cause of tooth loss in adults. This condition commonly begins as gingivitis where gums turn red and begin to swell and bleed, a situation experienced by too many people. Fortunately healthy gums and avoiding false teeth are both reasonable goals.
The elderly of today are much more likely to keep their teeth than previous generations. Even so, dental disease is prevalent. The New England Elders Dental Study found the beginnings of periodontal disease in over 3/4 of the 1150 persons examined. Part of the problem, said these investigators, was that education and dental care for this population are overlooked by both dentists and the patients themselves. The sad part of this situation is that proper dental hygiene and regular cleanings by the dentist are usually enough to stave off infection. Healthy people should replace their toothbrushes every two weeks; those with a systemic or oral illness more often. Everyone should use a new toothbrush when they get sick, when they feel better and again when they completely recover.
Myth: The older I get, the sicker I’ll get
It’s true that as we age, our physiology changes. These changes can lead to poor health if not addressed. But old age doesn’t have to mean feeling sick and tired. An important part of staying well into the older years is keeping your immune system operating at its peak. Aging is generally associated with lagging immunity and consequently more infections especially of the respiratory system. However, John Hopkins’ Professor Chandra discovered that when independent, apparently healthy, elderly people were fed nutritional supplements for a year, their immunity improved. Immunological responses were so marked that those who were supplemented (versus the placebo group) were plagued with less infections and took antibiotics for less days. Besides taking care of your immunity with supplementation, diet, exercise and other measures, you can prevent many age-related diseases with specific health precautions. For example, there is evidence that smoking and low plasma levels of vitamins C and E, and beta-carotene contribute to cataracts.
Calcium and magnesium supplementation helps some individuals with hypertension. Most are helped by high potassium foods (fruits and vegetables), salt restriction and weight maintenance. Keeping blood pressure under control can also decrease the risk of a stroke.
Adult-onset diabetes is usually treated best with dietary measures such as reducing simple sugars, consuming a lot of fiber and taking chromium supplements. It’s estimated that half of all types of cancer are linked to diet. This explains why less fat, lots of fruits, vegetables and fiber, vitamins A, B6, C and E and zinc and selenium all appear to play a role in cancer prevention.
Myth: Urinary incontinence is considered a normal part of aging
Although urinary incontinence (UI) occurs more frequently among older adults (10%–42% of hospitalized elders), it is not considered a normal part of aging and is highly treatable. A new onset of UI can signal problems such as urinary tract infection, electrolyte imbalances, mobility limitations, or medication side effects. Before beginning any rehabilitative interventions for incontinence, all possible causes should be investigated to rule out reversible factors. Bladder retraining for those with urge or stress incontinence is still highly effective for older adults. Behavioural management is the first line of treatment for incontinence.
Myth: Growing older means accepting the loss of independence and a Home for the Aged
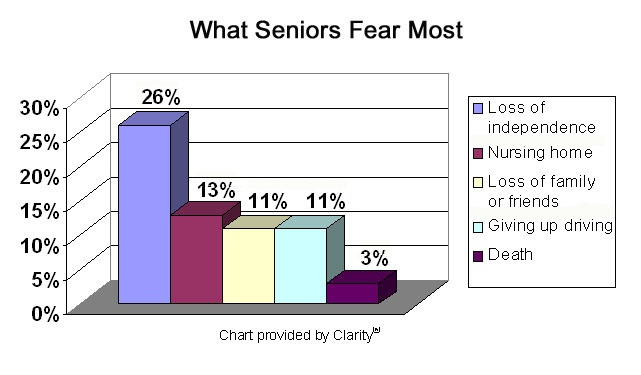
There is absolutely no evidence to support that as we age we accept loss of independence or going into a nursing home as part of the aging process. In fact today’s older adults enjoy a more vibrant and vigorous lifestyle. Remaining active, engaged and enjoying a more robust social life. An ever-increasing number of older adults are adopting home care in order to preserve the very things that the myth depicts. However, older adults do share common fears… in fact the 5 greatest noted fears among older adults are:
- Loss of independence
- Loss of loved ones
- Loss of friends
- Going into a Nursing Home
- Death
In Our Care supports the aging process so effectively that you never have to ever see the inside of Nursing Home, unless you’re visiting friends and family. We are fully equipped to handle all your care needs – Effectively, Efficiently & Affordably.

 A Summary of Canada’s Aging Population
A Summary of Canada’s Aging Population