Delirium
Delirium – Information for patients, families and Friends
It is our hope that this article will help you learn more about:
What is Delirium?
- The signs and symptoms
- How it can be prevented and
- What families, friends and caregivers can do to help
- Where to find more information
What is Delirium?

Delirium is a condition that causes a person to be confused. It is a physical problem (a change in the body) that can cause temporary change in the person’s thinking. Delirium usually starts over a few days and often get better with treatment.
Delirium can happen to anyone, anywhere. But, it often happens when someone is in the Hospital
Once identified, delirium is often treated as a medical emergency. Treatment is put in place right away because it can be a risk to patient safety.
Delirium can cause patients to slip and fall or to feel a lot of emotional and spiritual distress. A person with delirium may not be able to understand when people are trying to help them. They may become angry with family and hospital staff. They may start to think that everyone is against them or are trying to harm them. Some people with delirium may want to call the police to get help.
Delirium is like being in the middle of a very strange dream or nightmare, but the person is having these experiences while they are fully awake.
What is the risk of delirium?
- About 20 out of 100 patients admitted to hospital will experience.
- About 70 patients out of 100 admitted to the intensive care unit will experience delirium.
What causes delirium?
Delirium can be caused by:
A Physical illness (that brought someone to the hospital)
- Someone who is ill can have changes in their body chemicals, become dehydrated (not enough water in the body) or get an infection, such as a bladder infect or urinary tract infection. These kinds of problems can cause delirium.
Medications
- The medications the hospitals use to treat illness or control pain can cause delirium
Is delirium the same as depression or dementia?
No. Delirium can happen more often in people who have dementia or depression, but it is different.
Delirium happens quickly. It can come and go at any time. This does happen with dementia and depression.
Patients with delirium cannot focus their attention. This is different from patients with dementia and depression.
Types of Delirium
There are 2 types of delirium:
-
Hypoactive delirium
This type of delirium happens most often in elderly patients but can affect anyone at any age.
Patients with hypoactive delirium may:
- Move very slowly or not active
- Not want to spend time with others
- Pause frequently when speaking or not speak at all
- Look sleepy
-
Hyperactive delirium
This type of delirium is easier to recognize.
Patients with hyperactive delirium may:
- May be worried and afraid
- Be restless (not able to stay still or have trouble sleeping)
- Repeat the same movement many times
- Experience hallucinations (seeing something or someone that is not really there).
- Experience delusions (believe something that is not true).
At times a patient can have both hypoactive and hyperactive symptoms.
What are the signs and symptoms of delirium?
A check list:
Disorganized thinking YES NO
Saying things that are mixed up or do not make sense
Difficulty concentrating YES NO
Easily distracted or having difficulty following what is being said
Memory changes YES NO
Not able to remember names, places, dates, times or other important information
Hallucinations YES NO
Seeing or hearing things which are not real
Having delusions YES NO
Thinking or believing things which are not true or real
Feeling restless . YES NO
Not able to stay still, trouble sleeping, getting out of bed
Changing energy levels YES NO
Changes from being restless to being drowsy or sleepier than usual
How can delirium be prevented?
All patients should be carefully screened (checked) for these factors that may cause delirium:
- Hearing problems
- Vision problems
- Not enough water in the body (dehydration)
- Not being able to sleep or other sleep problems
- Dementia, depression or both
- Difficulty getting up and walking around
- Medication being taken
- History of alcohol or recreational drug use
- Chemical changes or imbalances in your body
- Low oxygen in your body
- Other health condition or illness
Having trouble:
- Thinking clearly, reasoning, remembering and judging
- Concentrating
- Understanding
- Express ideas
How is delirium be treated?
- The health care team helps the patient stay safe and calm
- They will try to find the cause of the delirium. Often, there is more than one cause. They also make sure any factors they find are not caused by another medical condition
- Then they will address the factors or ease the symptoms.
This could include:
- Reviewing and changing medications
- Provide fluids to rehydrate
- Correcting chemical problems in the body
- Treat infections
- Treating low oxygen levels
What can family and friends do to help?
Family and friends and caregivers can all help to prevent delirium for their loved ones in hospital.
Keep a careful watch for the signs and symptoms of delirium
- If you see any signs that could mean delirium talk with your health care team right away. Family members are often the first to notice these small changes.
- Use the signs and symptoms check list and factors list listed on this article to guide your findings.
Help with healthy eating and drinking while at the hospital
- Ask what is right for your loved one before they eat and drink.
- Make sure they have their dentures (if needed).
- Encourage help with eating. Feel free to bring their favourite foods from home, check with the health care team about foods they should not eat.
- Encourage them to drink often, if that is right for them.
Keep track of medications
- Share a complete list of their prescriptions and any over the counter medications they take with the health care team… including the dosage.
Help with activity
- Ask what is right for your loved one before starting any activities.
- Talk to the team about helpful and safe activities.
- Help them sit, stand and walk.
Help with mental stimulation
- Make a schedule for family and friends to visit. This will help your loved one feel safe and comforted.
- Speak to them in a calm, reassuring voice.
- Tell them where they are and why they are there throughout the day. If possible, place a large sign in their room or write information on it.
- For example, you could write: Today’s date, weather, where they are and their room number… this will help them stay connected.
- Give them instructions one at a time. Do not give too much information at once.
- Bring a few familiar objects from home, such as photo albums and their favourite music. If your loved one needs special care to prevent the spread of infection, check with the care team first.
- Open the curtains during the day time.
- Talk about current events.
- Read the newspaper out loud or use talking books
Help them with eyesight and hearing
- Make sure they wear their hearing aids or glasses, if they need them.
- Make sure there is enough light in the room.
- Help them use a magnifying glass, if they need one.
Help them rest and sleep
- Reduce noise and distraction.
- Soothe them with handholding, a massage, a warm drink or music.
- Bring a night light, but check with the health care team first.
- Use comfort items like their favourite pillow and blanket.
- Limit the number of visitors who come to see your loved one until the delirium goes away.
- The health care team may not give your loved one sleeping medications because it could make delirium worse.
Take care of yourself
It is not easy to be with a person with delirium, even though you may understand the problem
- Make sure to look after yourself and get some rest. Go out for short walks, remember to eat and drink fluids to keep up your energy levels.
- It may help to share your thoughts and feelings with someone. Feel free to speak with the health care team.
- Try not to become upset about the things your loved one may say during their delirium state. People with delirium are not themselves. In many cases, they will not remember what they said or did.
Who can I talk to if I have more questions or concerns?
There are many members of the health care team who can offer help and support. Talk with your doctor or nurse and any member of the health care team, including a Psychiatry, Spiritual Care or Social Work departments. They will answer any questions or concerns you may have about delirium.
Delirium should go away or be greatly reduced with the right kinds of treatment… although in some cases some of the symptoms may remain for an extended period of time.
More information can be found on these helpful websites:
Delirium Mayo Clinic www.mayoclinic.com/health/delirium/DS01064
Delirium MedlinePlus www.nlm.nih/gov/medlineplus/delirium.html
Videos:
Youtube – How to recognize Delirium www.youtube.com/watch?v=hwz9M2jZi_o
Many other videos choices will be available when you log on to this site.


 This article delves into ageist stereotypes dressed-up in the garb of myth that biases perceptions and experiences of being old. The article argues current ”mythmaking” about aging perpetuates that which it intends to dispel: ageism. It considers how traditional myths and folklore explained personal experience, shapes social life, and offers meaning for the unexplainable. The current myths of aging perform these same functions in our culture; however, they are based on half-truths, false knowledge, and stated as ageist stereotypes about that which is known. Recent studies in the cognitive sciences are reviewed to provide insight about the mind’s inherent ability to construct categories, concepts, and stereotypes as it responds to experience. These normal processes need to be better understood, particularly regarding how social stereotypes are constructed. Finally, the article argues that ageist stereotypes when labeled as ”myth” even in the pursuit of the realities of aging, neither educate the public about the opportunities and challenges of aging nor inform social and health practitioners about the aged.
This article delves into ageist stereotypes dressed-up in the garb of myth that biases perceptions and experiences of being old. The article argues current ”mythmaking” about aging perpetuates that which it intends to dispel: ageism. It considers how traditional myths and folklore explained personal experience, shapes social life, and offers meaning for the unexplainable. The current myths of aging perform these same functions in our culture; however, they are based on half-truths, false knowledge, and stated as ageist stereotypes about that which is known. Recent studies in the cognitive sciences are reviewed to provide insight about the mind’s inherent ability to construct categories, concepts, and stereotypes as it responds to experience. These normal processes need to be better understood, particularly regarding how social stereotypes are constructed. Finally, the article argues that ageist stereotypes when labeled as ”myth” even in the pursuit of the realities of aging, neither educate the public about the opportunities and challenges of aging nor inform social and health practitioners about the aged.


 A Summary of Canada’s Aging Population
A Summary of Canada’s Aging Population



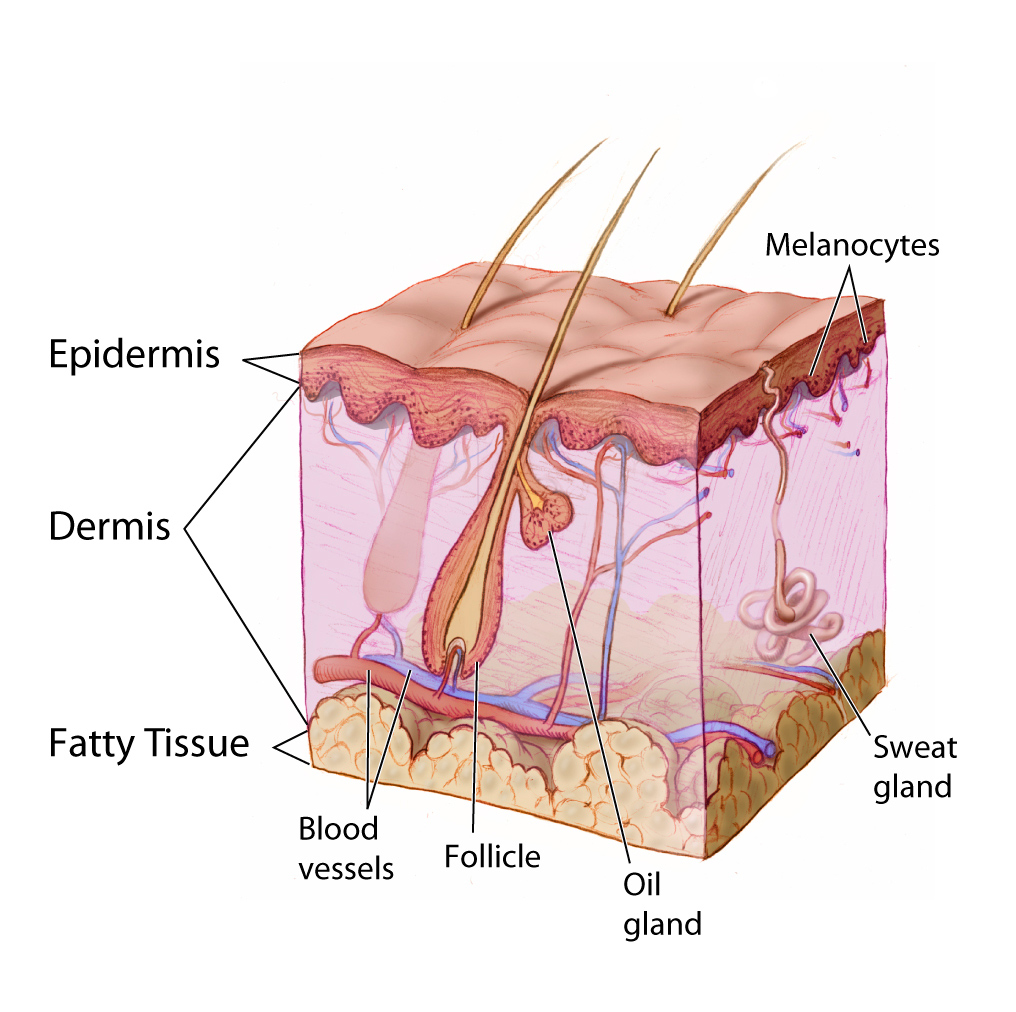 The importance of skin integrity as we age.
The importance of skin integrity as we age. What is Dementia?
What is Dementia?