A Summary of Canada’s Aging Population
 A Summary of Canada’s Aging Population
A Summary of Canada’s Aging Population
An aging Canadian population is expected to present significant social, economic and political challenges over the next decades. Understanding the needs of seniors and addressing the barriers they face can promote successful aging and ensure that Canadian society benefits from the numerous contributions seniors can provide as engaged citizens and voters.
This research note is the first in a two-part series on seniors, defined as those aged 65 and older. This note provides a demographic profile of this age group, including information about their geographical distribution, lifestyles and socio-economic status. It also addresses some of the challenges that they face in various areas of life. The second note will focus on the electoral participation of seniors, including turnout in federal elections, barriers to voting and initiatives that can be put forward to reduce these barriers.
The qualifying age for seniors is generally 65 in developed countries. However, seniors do not represent a homogenous group, and there is significant variation in the circumstances of those aged 65 to 74, 75 to 84, and 85 and older. Therefore, each one of these three age categories will be treated as distinct where possible.
The Aging Population
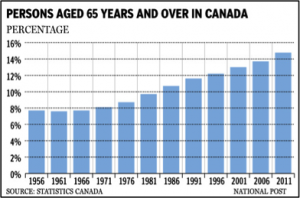
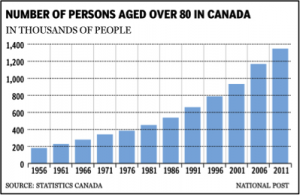
A sustained decline in mortality and fertility rates during the twentieth century has resulted in a shift towards older populations worldwide. Canada, while somewhat younger than the average among developed countries, still has an all-time high proportion of seniors. According to Statistics Canada, between 1981 and 2011, the number of Canadians increased significantly amongst the three age groups:
- For those aged 65 to 74, from 1.5 million (6% of the total population) to 2 million (8%)
- For those between 75 and 84, from 695,000 (2.8%) to 1.6 million (4.9%)
- For those aged 85 and older, from 196,000 (0.8%) to 492,000 (2%)
The number of seniors in all age groups is expected to continue to rise, and by 2041, seniors are projected to comprise nearly a quarter (24.5%) of the Canadian population, as compared to 14.8% today. Those aged 85 and over are expected to nearly triple to 5.8% of the total population by 2041.
The chart below illustrates the growth of the older population since 1921.
 Geography
Geography
Canada’s senior population is distributed unevenly across the provinces, with the highest concentration in the Atlantic provinces. Nova Scotia has the highest proportion of seniors, at 16.6% of its population, followed by New Brunswick (16.5%) and Prince Edward Island (16.3%). Alberta has the lowest proportion of seniors at 11.1% of the population, while Nunavut has the youngest population overall, with only 3.3% over 65. Some regions are aging more rapidly than others. The Atlantic Provinces are expected to see the highest increase in their proportion of seniors by 2026, while Ontario has the lowest projected increase. Most older seniors (61%) live in metropolitan areas, reflecting the overall trend towards urbanization in Canada, while 23% reside in rural areas.
Gender and Ethnicity
Since women have a longer life expectancy, the majority of seniors are women, with the gender discrepancy increasing with age. In 2011, women made up 52% of seniors aged 65 to 74, 56% of seniors aged 75 to 84, and 68% aged 85 or older. This gap is narrowing, however, and the next decades are expected to see a relative increase in the number of older men as they catch up in terms of life expectancy.
Approximately 28% of seniors are immigrants, the majority of whom were born in Western Europe and Asia. Most immigrant seniors moved at a relatively young age and have been living in Canada for several decades. The proportion of Aboriginal seniors is low, with only 5% of the Aboriginal population over 65, and 1% over 75.
Living Arrangements
As shown in table 1: Most people over 65 reside at home, either with a spouse or alone. According to a study released in 2002 by Health Canada, three quarters of seniors enjoyed housing considered to be affordable, adequately sized and in good condition.
A small percentage of seniors live in institutions, including long-term care facilities and hospitals, though rates of institutionalization rise sharply with age. Reasons cited for institutionalization include increasing frailty and care needs that exceed the capacity of family or friends. In many cases, family and friends continue to provide care even after institutionalization.
Table 1: Where Seniors Live
Living Arrangements |
% Of SeniorsAged 65–74 |
% Of SeniorsAged 74–85 |
% Of SeniorsAged 85+ |
Institution |
2.2 |
8.2 |
31.6 |
With Spouse |
54.4 |
39.9 |
16.2 |
With Children or Grandchildren |
18.9 |
16.0 |
15.8 |
Alone |
21.5 |
33.0 |
33.7 |
Other |
2.9 |
2.8 |
2.6 |
Employment and Income
As of 2006, nearly 15% of men and 5% of women over 65 were participating in the workforce. A smaller percentage of seniors in the 75+ age group were still working, with labour force participation rates of 7.5% for men and 2.4% for women. Self-employment and higher levels of education are associated with a higher likelihood that a person will continue to work after 65.
Post-retirement sources of income among retired seniors include transfers (such as CPP/QPP, OAS, EI, GIS), pensions, RSP withdrawals and investment income. Older seniors are often mischaracterized as impoverished. While they generally have only half the income of working-age households, they are often able to support a similar standard of living. This is likely due to lower expenses (for example, no mortgage or expenses related to child provision) and higher savings from which to draw.
Consumption and spending remain steady through the working years up to age 70, and then begin to decline. It is likely that this decline is voluntary, as gift giving and savings remain unchanged. Older seniors may be less willing or able to spend money; they may be saving for anticipated health care costs or to leave money behind for relatives.
Income aside, work is also important in defining personal identity. The loss of full-time employment, therefore, may present challenges to retired seniors, including lowered confidence, loss of perceived prestige and loss of purpose. Participation in various groups or organizations can ease the transition, and new challenges like volunteer activities may restore a sense of purpose.
Health and Quality of Life
Improved medical technology and public health measures have provided Canadians with a longer life expectancy and quality of life than in the past. Nonetheless, chronic health conditions are widespread among seniors, with four out of five seniors residing at home having a chronic health condition of some kind. The most common of these conditions are arthritis or rheumatism, hypertension, (non-arthritic) back pain, heart disease and cataracts. Alzheimer’s disease and other forms of dementia also affect significant numbers of older seniors and are expected to present a major social and public health problem as the population ages. In 2008, 480,600 people, or 1.5% of Canada’s population, suffered from some form of dementia. This number is expected to rise to 1.13 million (or 2.8% of the Canadian population) by 2038. Most dementia sufferers are 75 years of age or older.
Many seniors also have a disability or activity restriction that requires them to seek assistance with various activities. One quarter of older seniors require help with housework, while one in ten need help with personal care activities, such as washing, dressing or eating. Most assistance is provided by immediate family members, although friends and professional caregivers may help as well. Limitations increase sharply after 85, with mobility, sight, hearing and cognition becoming more restricted.
Despite the prevalence of chronic conditions and activity limitations, seniors generally perceive themselves to be in good health. As of 2011, 46% of men and women over 65 rated their own health as very good or excellent. Higher levels of educational attainment are strongly related to better self-reported health, as are greater independence, the absence of pain or barriers to communication, and the presence of strong social networks. Even seniors residing in long-term care facilities generally rate their health fairly highly, suggesting that they adjust their expectations for health relative to their circumstances and those of their peers.
Victimization, Abuse and Ageism
Elder abuse is gaining increasing recognition as an important issue. Abuse can be physical, psychological/emotional, sexual or financial in nature, or involve intentional or unintentional neglect. A random survey of seniors in Canada found that 4% reported experiencing maltreatment since turning 65. Older women and sponsored immigrant seniors are particularly vulnerable to elder abuse. This could be due to increased financial dependency, social isolation, cultural norms, familial status, disadvantage or disability.
Fraud against older people is also common. Seniors may be particularly vulnerable due to isolation and, in some cases, cognitive decline. Types of scams may include mail or telephone fraud, charity or lottery scams, or fake business opportunities.
Older seniors may also experience a type of discrimination referred to as ageism, defined as a “process of systematic stereotyping or discrimination against people because they are old, just as racism and sexism accomplish with skin colour and gender.” Ageism may be positive (for example, the belief that all seniors are wise or caring) or negative (one study shows that younger Canadians overwhelmingly assume that most seniors reside in an institution, suffer from dementia and are responsible for a large proportion of traffic accidents). Ageism can have implications for individuals whose competencies and merits are not acknowledged, and for society as a whole, which, operating under the assumption that everyone is young, fails to meet the varied needs of all of its citizens.
What Older Seniors Fear The Most
A recent study looked at some of the fears that seniors experience as they age. Losing their personal independence and going into a Nursing Home were among the their greatest fears… more so than death.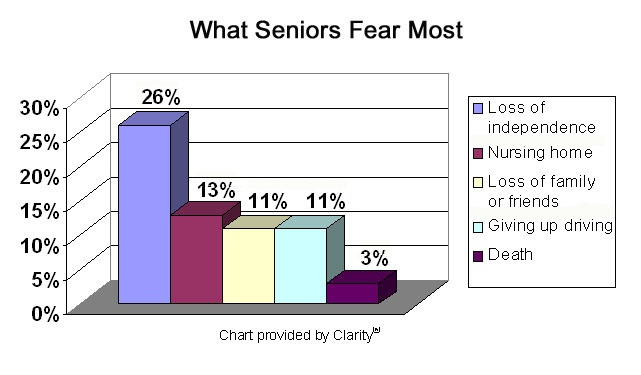
Social and Civic Participation
It is important for seniors to remain active in social networks, as this fosters a sense of belonging and connectedness, and is associated with better health and quality of life outcomes. Seniors who are socially involved are less isolated and tend to have more close friends.
As of 2003, 54% of seniors were involved in groups or organizations, such as social clubs, service clubs, sports leagues and religious organizations. This proportion is similar to that of adults under 65. For seniors over 75, the rate of group involvement dropped to 46%. Seniors with higher levels of education and those with a previous history of involvement are more likely to participate in a group or organization.
Many seniors also volunteer for charities or non-profit organizations. While they are somewhat less likely to volunteer than younger retirees or working people, they tend to contribute more hours when they do volunteer. In 2004, 39% of seniors between 65 and 74 volunteered, contributing an average of 250 hours of volunteer work – 100 hours more than the average for adults between 25 and 54. Volunteering decreases somewhat after age 75, health being the most widely reported reason for non-volunteering seniors.
Conclusion
The role of seniors in society warrants increased consideration as their share of the population grows. Currently, seniors have a good quality of life in Canada. Most enjoy good living conditions, adequate financial resources, and generally rate their health highly. While the majority of seniors are retired, many remain socially involved through participation in organizations or volunteer work. Nonetheless, seniors continue to face certain challenges and barriers. These include physical and cognitive health conditions, a lack of independence and negative attitudes.
Understanding the needs of seniors and addressing the barriers they face can promote successful aging and bring benefit to Canadian society from the numerous contributions older people can provide, including their participation in the electoral process.
Please contact us today, to discuss any challenges you may be facing and how our services can help you remain independent, protected, safe, and in you home / community.
You got questions, we have answers: (905) 785-2341 or email us at homecare@inourcareservices.com