Senior Care: Elderly Suicide

Loneliness & depression can bring on other challenges
The Elderly and Suicide
So we’ve all heard of depression. We even seem to be aware of what causes it & how to overcome it, but do we really?
So what’s the big deal with depression? The deal is…
In 2011 statistical report stated that someone over the age of 65 commits suicide every 90 minutes (16 deaths per day). In 2013 it was reported that this statistic had doubled. Elders, account for one-fifth of all suicides, but it only represents 12% of the population. White males over the age of 85 are at the highest risk and completion of suicide attempts, almost six times the national average. The suicide rate among elders is two to three times higher than in younger age groups. Elder suicide may be under-reported by as much as 40% or more. Omitted are “silent suicides”, i.e., completions from medical noncompliance and overdoses, self-starvation or dehydration, and “accidents.” The elderly have a high suicide rate because they use firearms, hanging, and drowning. The ratio of suicide attempts to completions is 4:1 compared to 16:1 among younger adults. “Double suicides” involving spouses or partners occur most frequently among the aged. Elder attempters have less chance of discovery because of greater social isolation and less chance of survival because of greater physical frailty and the use of highly lethal means.
What are the causes?
Elder suicide is associated with depression and factors causing depression, e.g., chronic illness, physical impairment, unrelieved pain, financial stress, loss and grief, social isolation, and alcoholism. Depression is tied to low serotonin levels. Serotonin, is a neurotransmitter in our brains that regulates and limits self-destructive behaviour. As we age our Serotonin levels decrease placing us at greater risk. Depression remains under diagnosed and undertreated among the elderly population.
What are some of the key risk factors of elder suicide?
- Loss of spouse.
- A late onset depressive disorder.
- A debilitating and/or terminal illness.
- Severe chronic/intractable pain.
- Decreasing independence and self-sufficiency.
- Decreased socialization and social supports.
- Risk often accumulates among the elderly. An individual may be white, male, and an alcohol user and then become a widower or depressed.
What are some of the myths of elder suicide?
- It is the outcome of a rational decision and justified.
- Elder victims are usually seriously or terminally ill.
- Only very severely depressed elders are at risk of suicide.
- Suicidal elders never give any indication of their intent.
- The suicide of an older person is different from that of a younger individual.
What are the warning signs?
The following may indicate serious risk:
- Loss of interest in things or activities that are usually found enjoyable
- Cutting back social interaction, self-care, and grooming.
- Breaking medical regimens (e.g., going off diets, prescriptions)
- Experiencing or expecting a significant personal loss (e.g., spouse)
- Feeling hopeless and/or worthless (“Who needs me?”).
- Putting affairs in order, giving things away, or making changes in wills.
- Stock-pilling medication or obtaining other lethal means
Other clues are a preoccupation with death or a lack of concern about personal safety. “Good-byes” such as “This is the last time that you’ll see me” or “I won’t be needing anymore appointments” should raise concern. The most significant indicator is an expression of suicidal intent.
Why aren’t community agencies or providers doing more service involvement with older men?
Community agencies basically serve elderly women who have a suicide rate well under the national mean for all ages. Community agencies may be little concerned because elder suicide is uncommon in their caseloads.
Agency philosophy:
The prevailing value in most services for the aged is to optimize self-sufficiency in terms of individual capability and safety. A commitment to autonomy may cause community agencies to let the client or patient control decisions on referrals to other resources, alerting relatives, or involving available services.
Agency Misconceptions:
- Community agencies and providers may accept some of the myths about suicide such as:
- If someone’s determined to commit suicide, no one can stop him or her.
- Those who complete suicide do not seek help before their attempt.
- Those who kill themselves must be crazy.
- Asking someone about suicide can lead to suicide.
- Pain goes along with aging so nothing can be done.
- It makes sense for an old person to want to end their suffering.
- Old people are used to death and loss and don’t feel them like younger folks.
- Those who talk about suicide rarely actually do it.
- How many health or human service professionals, other staff, and volunteers believe these statements to be true?
Lack of risk assessment:
A lack of attention to elder suicide and a concentration on client or patient self-determination and self-sufficiency may limit community agencies’ response. Most community agencies do not recognize the problem and consequently do little or no screening for it among their clientele.
What can community agencies do?
Individual prevention must focus on what drives suicide. “Doing something” basically comes down to caring. Community level prevention of late life suicides will require “creative partnerships of primary care providers. This means that senior centers, home care providers, hospices, adult day care, home-delivered meals programs, para-transit, and other organizations serving the elderly are going to have to team up with community mental health centers. This must start soon as the high-risk segment of the aged population is growing rapidly and the oldest baby boomers are within a few years of turning 65. The boomers will arrive in their “golden years” having manifested higher suicide rates on the way than prior generations.
If you think… This cannot be happening here in Canada, Think again!
Canada’s elderly are at high risk of suicide experts say, and Canadian men aged 85 to 89 have the highest rate of suicide. THE CANADIAN PRESS: Dr. Marnin Heisel says public awareness about suicide lets people know their physical and mental health problems can be treated effectively. Studies show that Canada’s elderly are at a much higher risk of suicide than adolescents, and there is growing concern among mental health experts that psychological care may be out of reach for most seniors. Dr. Marnin Heisel, a clinical psychologist and professor at the University of Western Ontario, says lack of public awareness of the issue is a key problem that affects not only the elderly but also their families and the public in general.
“One of the challenges that people face is thinking ‘I’m unique in this, I’m alone, there’s something wrong with me, no one can understand it,’ and then they tend to back away from family, other supports, including professional supports” Heisel said in an interview.
Public awareness lets the people struggling with these issues know that they are not alone and their physical and mental health problems can be treated effectively, he said. It may also cue their relatives into the fact that their older family members who are struggling with depression might be contemplating suicide, he said. “They might, as a result, begin asking their family (member) ‘How are you doing? Are you struggling with some of these things?’ or even asking them if they’ve thought of suicide.” A 2009 report by Statistic Canada states that men aged 85 to 89 have the highest rate of suicide among any age group in Canada, at a rate of about 31 per 100,000, and usually do so through more violent means. A report by the chief public health officer released the following year also showed that men over the age of 85 have on average higher suicide rates than all other age groups. For most Canadians, psychological services — which can easily run $100 or $200 an hour — are not covered by provincial and territorial health-care plans, but psychiatric services and medications generally are. Psychological care is covered only if it’s hospital-based. “But many if not most hospitals, at least in Ontario, typically don’t have very much in the way of psychological services and typically not for older adults,” said Heisel. “One thing we do know is that unless somebody has extremely good third-party health coverage, or they are a child in the school system, or a veteran, or if they have access to psychological services as a result of a motor vehicle collision — most Canadians can’t access psychological services unless they pay out-of-pocket. Heisel says research has shown that 75 per cent of older adults who die by suicide had seen a primary-care physician or provider within a month prior to ending their lives. “That suggests that primary care is a key place where we should be assessing for screening for suicide risk factors and then try to implement aggressive, meaning very focused, interventions,” Heisel said. “And we really don’t see that happening, literature supports that treatments works extremely well; it just requires funding to do that.” There’s also concern that many elderly suicides go undetected due to the way they are reported by coroners across Canada. “I can envision a circumstance, for example, where an elderly male is found (deceased) in a bed alone … maybe with no history of depression or suicidal thinking that he had expressed to anybody, and the coroner could determine that the death was due to natural causes and not even order an autopsy because of the age group,” said Dr. William Lucas, Ontario deputy chief coroner for inquest. “And if the person had used a relatively subtle means like an overdose of medications … that wasn’t obvious … we wouldn’t know,” he said. Heisel says research shows that when the means of death are more ambiguous, then suicide is more likely not to be detected. He goes on to say, “It’s somewhat frustrating because we really don’t know the full scope of the issue”. The frustration stems from the fact that many suicide prevention strategies are largely aimed at youth. That’s why he says he decided to speak publicly about the issue. Victims of depression say that family is what helps them the most in combating episodes of depression, in addition to staying physically active, mentally stimulated, including social companionship in their daily lives with interaction in the community. “Those are the good things in life when periods of depression start to creep in”. Incorporate them to combat depression and from recurring episodes. One patient says… “Well if the glass is half empty, it must be half full … I try to forget about the half-empty side but what a wonderful half full my life is.” The following posted articles also speak to this issue in the same relative terms… it a bigger problem that we think and about to get bigger. Be sure to also read the posted comments from readers, as it further illustrates the issue in the elderly communities. Suicide rates climb among elderly in Canada. Elderly suicide rates hitting new highs as traditional social networks break down. Over the past years our aging population has skyrocketed. This growth is only expected to increase exponentially over the next 15-20 years. The issues we are currently facing and learning about are just the beginning of the cycle. Growing challenges relating to care of our elderly will continue to provoke our ideals of what is acceptable in our society. Anything that we have an answer for (treatment) is therefore a preventable measure… like the treatment for depression and respectively reduce depression related suicides.
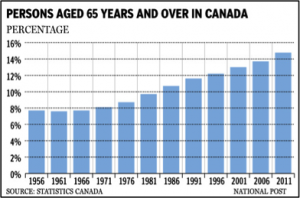
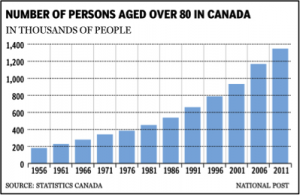
The following graphs illustrate the population growth for the following demographics.
For a more detailed population projection statistical review visit the Canadian Statistics web page.
It is within us to create an environment whereby our elders are cared for in a manner that protects them physically & holistically, paving the way for the future. Our campaign and advocacy to enriching the lives of our elderly should be one of our primary goals… “We ourselves are becoming to ones who will require care in the near future and our actions today will dictate the outcome for ourselves tomorrow”.

 What is Dementia?
What is Dementia?