 What is Osteoporosis?
What is Osteoporosis?
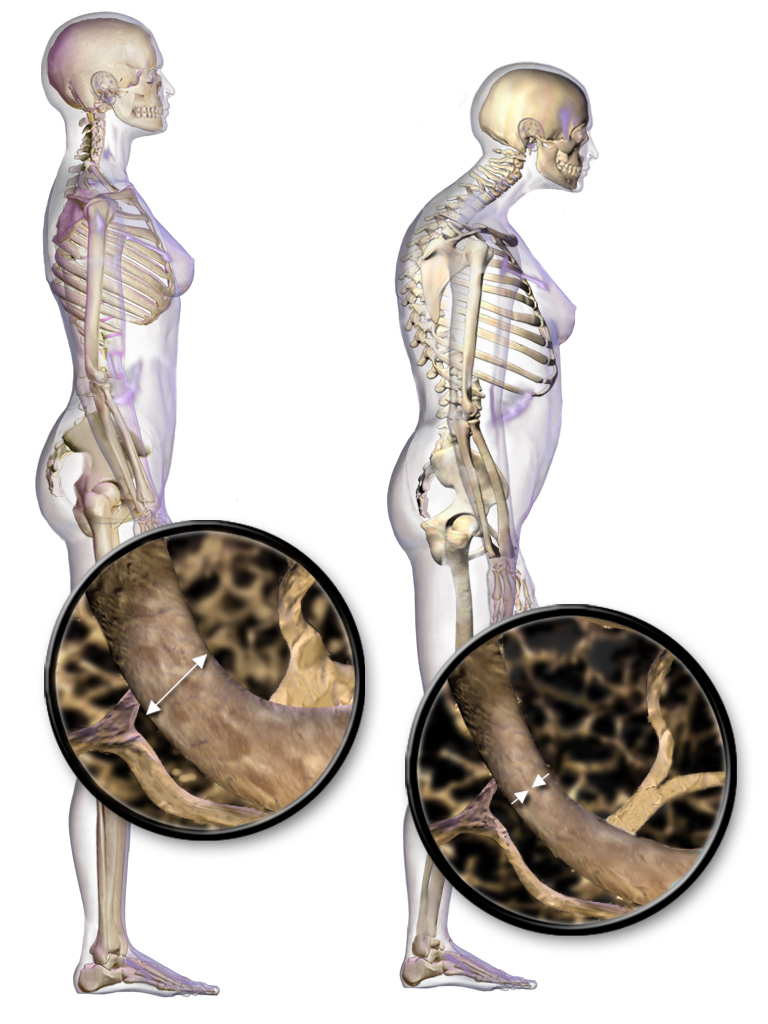
Osteoporosis is a disease characterized by low bone mass and deterioration of bone tissue. This leads to increased bone fragility and risk of fractures, particularly of the hip, spine, wrist and shoulder. Osteoporosis is often known as “the silent thief” because bone loss occurs without symptoms.
Osteoporosis is sometimes confused with osteoarthritis, because the names are similar. Osteoporosis is a bone disease; osteoarthritis is a disease of the joints and surrounding tissue.
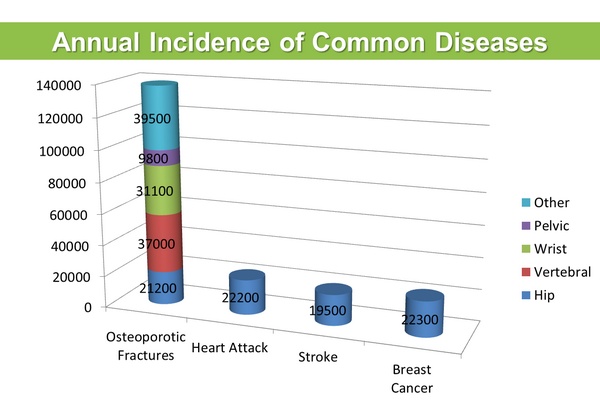
PREVALENCE Fractures from osteoporosis are more common than heart attack, stroke and breast cancer combined.
At least one in three women and one in five men will suffer from an osteoporotic fracture during their lifetime.
COSTS The overall yearly cost to the Canadian healthcare system of treating osteoporosis and the fractures it causes was over $2.3 billion as of 2010. This cost includes acute care costs, outpatient care, prescription drugs and indirect costs. This cost rises to $3.9 billion if a proportion of Canadians were assumed to be living in long-term care facilities because of osteoporosis. The reduced quality of life for those with osteoporosis is enormous.
Osteoporosis can result in disfigurement, lowered self-esteem, reduction or loss of mobility, and decreased independence. The statistics related to hip fractures are particularly disturbing. There were approximately 25,000 hip fractures in Canada in 1993. Twenty-eight per cent of women and 37% of men who suffer a hip fracture will die within the following year. Over 80% of all fractures in people 50+ are caused by osteoporosis.
ABOUT OSTEOPOROSIS Osteoporosis is a condition that causes bones to become thin and porous, decreasing bone strength and leading to increased risk of breaking a bone. As previously mentioned, the most common sites of osteoporotic fractures are the wrist, spine, shoulder and hip.
- No single cause for osteoporosis has been identified.
- Osteoporosis can strike at any age.
- Osteoporosis affects both men and women.
- Osteoporosis is often called the ‘silent thief’ because bone loss occurs without symptoms unless one has fractured.
- Osteoporosis can result in disfigurement, lowered self-esteem, reduction or loss of mobility, and decreased independence.
- Osteoporosis has been called a paediatric disease with geriatric consequences.
Building strong bones during childhood and adolescence can be the best defence against developing osteoporosis later. Peak bone mass is achieved at an early age, age 16-20 in girls and age 20-25 in young men. Women and men alike begin to lose bone in their mid-30s; as they approach menopause, women lose bone at a greater rate, from 2-3 per cent per year.
Risk factors include age, sex, vertebral compression fracture, fragility fracture after age 40, either parent has had a hip fracture, >3 months use of glucocorticoid drugs, medical conditions that inhibit absorption of nutrients and other medical conditions or medications that contribute to bone loss. Loss of 2cm (3/4″) as measured by one’s healthcare provider or 6cm (2 1/2″) overall from when one was younger may be an indicator of spinal fracture. 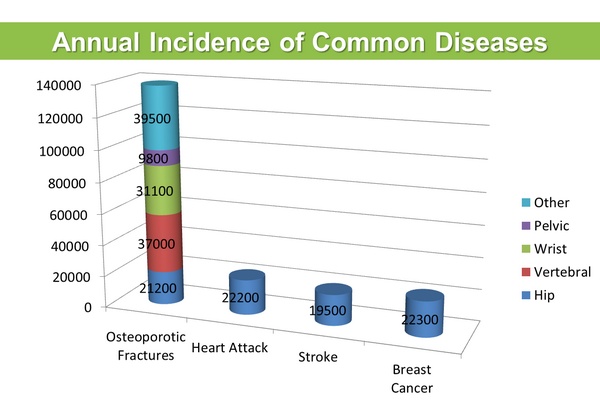
FACTS AND FIGURES
Each hip fracture costs the system $21,285 in the 1st year after hospitalization, and $44,156 if the patient is institutionalized. Osteoporotic hip fractures consume more hospital bed days than stroke, diabetes, or heart attack.
Fewer than 20% of fracture patients in Canada currently undergo diagnosis or adequate treatment for osteoporosis. Without BMD testing, 80% of patients with a history of fractures are not given osteoporosis therapies. Hundreds of thousands of Canadians needlessly fracture each year because their osteoporosis goes undiagnosed and untreated.
A study recently reported that only 44% of people discharged from hospital for a hip fracture return home; of the rest, 10% go to another hospital, 27% go to rehabilitation care, and 17% go to long-term care facilities. Persons with a wrist fracture (14%) suffered a repeat fracture within 3 years. One in three hip fracture patients re-fracture at one year and over 1 in 2 will suffer another fracture within 5 years. The risk of suffering a second spine fracture within the first 12 months following an initial vertebral fracture is 20%.
How strong are your bones? Assessing your risk and testing for bone loss are the keys to diagnosing osteoporosis. Osteoporosis is a potentially crippling disease characterized by low bone mass (density) and deterioration of bone tissue. Osteoporosis does not develop overnight. You can lose bone mass steadily for many years without experiencing any symptoms or signs of the disease until a bone fractures.
For this reason, osteoporosis is often called “the silent thief” – literally stealing our bone mass without giving us any indication whatsoever. If osteoporosis is first diagnosed at the time a fracture occurs, it is already fairly advanced. Early detection of bone loss, therefore, is critical in preventing osteoporotic fractures. This section is designed to help you assess your risk of osteoporosis so that you may take preventive action.
Osteoporosis and Osteoarthritis Despite the fact that osteoporosis, arthritis and osteoarthritis (a form of arthritis) are completely different conditions, they are frequently confused, in particular osteoporosis and osteoarthritis, because both names start with “osteo.”
| |
Osteoporosis |
Osteoarthritis |
| Definition |
Osteoporosis is a bone disease. The word “osteoporosis” literally means porous bones. It is a bone disorder characterized by decreased bone strength as a result of reduced bone quantity and quality. A person with osteoporosis has an increased risk of breaking a bone (fracturing) easily. |
Osteoarthritis is the most common form of arthritis. It is a degenerative joint disease that involves thinning or destruction of the smooth cartilage that covers the ends of bones, as well as changes to the bone underlying the joint cartilage. Osteoarthritis produces pain, stiffness and reduced movement of the affected joint, which ultimately affects ones ability to do physical activities, reducing quality of life. |
| Symptoms |
Osteoporosis is called “the silent thief” because it can progress without symptoms until a broken bone occurs. When bones become severely weakened by osteoporosis, simple movements – such as bending over to pick up a heavy bag of groceries or sneezing forcefully – can lead to broken bones. Hip, spine and wrist fractures are the most common fractures associated with osteoporosis. |
Osteoarthritis most often affects the hips, knees, fingers (i.e., base of the thumb, tips and middle joints of the fingers), feet or spine. It affects each joint differently, and symptoms are easy to overlook. It can be painful – the pain may result from overuse of a joint, prolonged immobility or painful bony growth in finger joints. |
| Diagnosis |
Osteoporosis is diagnosed through a bone mineral density test, a simple, painless test that measures the amount of bone in the spine and hip. |
Osteoarthritis is diagnosed based on medical history, physical examination and x-rays of the affected joints. activities, reducing quality of life. |
| Risk Factors |
The risk of osteoporosis may be reduced by becoming aware of these risk factors and taking action to slow down bone loss. Low bone mineral density is a major risk factor for fracture, the main consequence of osteoporosis. Other key risk factors include older age, prior low-trauma fracture, a history of falls and use of certain medications, such as corticosteroids (for example, prednisone). Family history of a fragility fracture is often a contributing factor. |
Some factors that can contribute to the development of osteoarthritis include family history, physical inactivity, excess weight and overuse or injury of joints. |
| Treatment |
Osteoporosis can be treated with lifestyle changes and, often, the use of prescription medication. Paying attention to diet (adequate calcium and vitamin D intake) and getting regular physical activity are important lifestyle changes. Weight-bearing and strength training exercises can help to manage pain and improve the strength of bones and muscles, which helps to prevent falls. Broken hips caused by osteoporosis usually need to be repaired surgically. This can include the use of specialized “pins and plates,” but can also involve hip replacement surgery. This is determined by the surgeon based on the exact type of hip fracture that has occurred. If you have osteoporosis, there are effective medications that can reduce your risk of fracture. |
Osteoarthritis can be managed with the use of joint protection (decreasing the amount of work the joint has to do), exercise, pain relief medication, heat and cold treatments, and weight control. Severe arthritis may be treated with an operation, where damaged joints are replaced with an artificial implant. Knee and hip joint replacements are commonly performed. |
A few basic facts:
Osteoporosis is a bone disease in which the amount and quality of the bone is reduced, leading to fractures (broken bones). Osteoporosis produces no pain or other symptoms unless a fracture has occurred. Arthritis (arth = joint; itis = inflammation) is a disease of the joints and surrounding tissue. Osteoarthritis and rheumatoid arthritis are the most common forms of arthritis. A joint is the location at which two or more bones make contact and allows for movement of the bones. A person can have osteoporosis and osteoarthritis at the same time.
Both diseases may cause pain and limit mobility, but the cause of this pain and the way it is treated are quite different. An accurate diagnosis of your pain is very important. With an accurate diagnosis, you will be better able to develop a pain management program that works for you. The prefix “osteo” (which means “bone”) is the only thing that osteoporosis and osteoarthritis have in common.
IF YOU HAVE BOTH DISEASES
Individuals who suffer from osteoarthritis and osteoporosis should seek help planning a program to manage both conditions and pay special attention to advice about exercise. Regular weight-bearing exercise is usually recommended for individuals with osteoporosis, but may be difficult to follow in the presence of significant hip or knee arthritis. Keeping joints mobile requires a special approach to exercise and movement. A specially trained physiotherapist can help ensure exercises are safe and beneficial for both conditions.
WHERE TO GET HELP
Arthritis: The Arthritis Society (TAS) is the leading source of information on arthritis, including osteoarthritis. For more information about arthritis, contact:
The Arthritis Society
: 1-800-321-1433
www.arthritis.ca.
Osteoporosis: Osteoporosis Canada (OC) is the leading source of information on osteoporosis in Canada. OC provides individuals concerned about their risk of developing this disease and those who have been diagnosed with up-to-date information on all aspects of bone health. Information counsellors oare available at a toll-free line (1-800-463-6842).
Men and Osteoporosis
Osteoporosis is not just a woman’s disease. It is also a serious health issue for men. During their lifetime, at least one in three women and one in five men will suffer a broken bone from osteoporosis. Approximately 30,000 hip fractures occur in Canada each year, and over one quarter of these occur in men.
Proportionately more men than women die as a result of a hip fracture – 37% of men who suffer a hip fracture will die within the year following that fractured hip. Men are also more likely than women to require care in a long-term facility after a hip fracture. Yet despite the fact that hip fractures can be more devastating for men than for women, men are less likely to be assessed for osteoporosis or to receive treatment for osteoporosis after they break a bone.
Secondary Osteoporosis
Drugs and Diseases that can Cause Bone Loss, Falls and/or Fractures
There are several well known risk factors for osteoporosis and osteoporotic fractures such as age, sex, low body weight, a low bone mineral density, a past fragility fracture, having a parent who had a hip fracture and a past history of fall(s). Less well known are which medications and medical conditions can increase the risk of osteoporosis and osteoporotic fractures either by causing more thinning of bones, by increasing the risk of falls or both.
Osteoporosis that results from having another disease or condition or from the treatment of another condition is called secondary osteoporosis. This fact sheet will present a brief summary of the commoner causes of secondary osteoporosis.
How to Minimize the Harmful Effects
Talk to Your Doctor
This fact sheet may not include all medications or all medical conditions that can contribute to fractures. If you are taking any medications or suffer from any medical conditions that may increase bone loss or the risk of falls, talk to your doctor and request a fracture risk assessment, which is a more in-depth assessment of your bone health. To do this your doctor may suggest you have a bone mineral density (BMD) test. This is a painless test that can help to predict your likelihood of fracture. Your doctor will also need to consider other risk factors including your age, sex, fracture history, parental history of hip fracture and glucocorticoid use.
Calcium, Protein and Vitamin D
The Osteoporosis Canada (OC) fact sheet Nutrition: Healthy Eating for Healthy Bones can help you determine if you are getting enough calcium and vitamin D. OC recommends that as much as possible, calcium intake should be from food, and supplements should only be taken if one cannot consume sufficient calcium from the diet. On the other hand, there are few food sources of vitamin D and sun is an unreliable source, so OC recommends daily vitamin D supplementation all year round for all Canadian adults. A balanced diet, following Canada’s Food Guide, will ensure that you get sufficient protein and other nutrients essential for bone health.
Regular Exercise
Exercise helps build and maintain strong muscles and bones. The OC fact sheet Exercise for Healthy Bones provides good general guidelines for choosing the exercise that is right for you.
Smoking and Alcohol
Any type and amount of smoking contributes to bone loss and increases the risk of osteoporosis in both men and women. Drinking an average of three or more alcoholic beverages per day may also increase bone loss and fracture risk. OC recommends no smoking and no more than an average of two alcoholic drinks daily.
Checklist for Risk of Broken Bones and Osteoporosis
Part A:
□ Am I 65 or older?
□ Have I broken a bone from a simple fall or bump since age 40?
□ Has either my mother or father had a hip fracture?
□ Do I smoke?
□ Do I regularly drink three or more alcoholic drinks per day?
□ Do I have a condition that requires me to use a glucocorticoid medication such as prednisone?
□ Do I take any other medication that can cause osteoporosis such as an aromatase inhibitor for breast cancer or hormonal treatment (androgen deprivation therapy) for prostate cancer?
□ Do I have a medical condition that can cause bone loss or fractures? Examples include rheumatoid arthritis, celiac disease, gastric bypass surgery, COPD (chronic obstructive pulmonary disease) or chronic liver disease.
□ Did I have an early menopause, i.e. before age 45?
□ Have my periods ever stopped for several months or more (other than for pregnancy or menopause)?
□ Have I ever suffered from impotence, lack of sexual desire or other symptoms related to low levels of testosterone (male sex hormone)?
□ Do I currently weigh less than 60 kg or 132 lbs?
□ Have I lost more than 10% of my body weight since age 25?
□ Have I recently had an X-ray that showed a spinal fracture?
□ Have I had an X-ray that showed low bone mineral density?
If you are over 50 and have checked one or more of the above, Osteoporosis Canada recommends that you talk to your doctor to see if you need a bone mineral density test and about doing a comprehensive fracture risk assessment with FRAX or CAROC.
If you are under 50, it is very unlikely that you need a bone mineral density test unless you have a chronic medical condition or medication that puts you at high risk for fractures. If you are unsure, speak to your doctor.
Part B:
□ Have I lost 2 cm (3/4″) in height as measured by my healthcare provider, or 6 cm (2 1/2″) overall from when I was younger?
□ Do I have kyphosis (a forward curvature of the back)?
If you are over 50 and have checked one or more of the above, Osteoporosis Canada recommends that you talk to your doctor about getting checked for the possibility of a spine fracture. This is done with a regular back X-ray.
Part C: Frequent falls can lead to broken bones.
□ Have I fallen two or more times in the past year?
□ Do I have an unsteady walk and poor balance? □ Do I need to push with my arms to get up from a chair?
□ Do I need an assistive device such as a cane, walker or wheelchair? If you have checked one or more of the above, you are at risk of falling and you need to take steps to prevent falls.
Nutrition – Healthy eating for healthy bones
As we get older, we often pay less attention to our diet. We may live alone and not always bother cooking a meal. We may become less active as we age, which can also reduce our appetite. Grocery shopping may become more difficult so we do less of it. The result is that we soon run out of items like milk, yogurt and fresh fruit and vegetables. The next thing you know, some tea and toast is all we really have left, or care to prepare. It is important to plan your diet and your grocery shopping so that your bones will stay as healthy and strong as possible. You have no doubt heard that calcium and vitamin D are good for your bones.
They are, but they are not the only important nutrients. A well balanced diet, made up of all the four food groups in Canada’s Food Guide, is the secret to healthy bones.
MEAT AND ALTERNATIVES
In addition to calcium and other minerals, bone is made up of protein, a nutrient that is necessary for building and repairing body tissues including bones. Protein gives bone its strength and flexibility. Protein is also the big component of muscles, which are, of course, crucial for mobility and in preventing falls. The “Meat and Alternatives” food group provides your body with protein. Meat and alternatives also contain other vitamins and minerals that are essential for overall good health.
How do you know how much protein you need? Canada’s Food Guide recommends 2 – 3 servings of meat or alternatives each day for those over 50. A serving size is about the size and thickness of your palm (excluding the thumb and fingers). This means that you should eat a palm size portion of protein with at least two of your three meals. The “Meats” include beef, pork, poultry and fish. The “Alternatives” include beans, lentils, tofu, egg whites, peanut (or other nut) butters, shelled nuts and seeds. Dairy products are also a good source of protein and have the added advantage of being good sources of calcium.
Too many seniors don’t eat enough protein or other important nutrients. Less protein means more fragile bones. Less protein also means weaker muscles. Weaker muscles lead to poorer balance and more falls, and falls can lead to fractures. It is not unusual to find that people who break a bone also had a deficiency of protein in their diet over a period of several months just before their fracture. So, put ham or peanut butter on your morning toast; have boiled eggs or a salmon sandwich with your lunch, a chicken breast or hamburger patty with your supper. Eat well and eat regularly. Exercise for Healthy Bones
WHY SHOULD I EXERCISE?
Regular exercise improves health in many ways. People who engage in regular exercise have lower rates of depression, heart disease, dementia, cancer, diabetes and many other chronic diseases. Exercise can improve physical fitness, strength, energy levels, stamina and mental health. In children and teens, frequent and vigorous exercise helps to increase bone strength. In older adults, certain types of exercise help to prevent bone loss.
Exercise also improves balance and coordination, which helps prevent falls and this in turn may reduce fractures. Exercise is very important for all, but especially for those with osteoporosis and those who are at risk of a broken bone (fracture) caused by osteoporosis. Because everyone is different, it is impossible to develop a “one size fits all” program for exercise.
WHAT EXERCISES ARE SAFE AND APPROPRIATE FOR ME?
The first step is to consult your doctor before you start a new exercise program. Any exercise may carry with it a certain amount of risk. If you have osteoporosis or low bone mass, or have broken a bone from a minor event such falling from a standing height or doing a simple task, you must be aware of yourfracture risk to determine the specific types of exercises that you can perform safely and those you should avoid.
A comprehensive fracture risk assessment will tell you if you are at low, medium or high risk of fracture. This in turn will assist your doctor and your physiotherapist in designing an exercise program that is safe and most beneficial for you, and identifies the precautions you need to take. A comprehensive fracture risk assessment does not rely solely on the results of a bone mineral density (BMD) test. The assessment begins with your doctor asking you questions about your past medical history, including whether or not you broke any bones and how those fractures happened, as well as questions about your family’s medical history. He/she may also examine you and send you for tests that may include blood tests and/or a bone mineral density test.
Your doctor may also order an X-ray of your spine to make sure you don’t have any spine fractures because two-thirds of spine fractures are “silent,” meaning they do not cause any pain. If you have a spine fracture from osteoporosis, this means that your risk for another fracture is high. It also means that you should avoid high impact exercises or sports that require forward bending, heavy lifting, reaching overhead, twisting, jumping, bouncing or jerky movements.
What Types of Exercise Should I Do?
A comprehensive exercise program includes all of the following:
- weight-bearing exercise
- strength training exercise
- posture training
- balance training and
- stretching
Although most individuals can perform all five types of exercise, some exercises may need to be modified for those who have a moderate or high risk of fracture, including those with spine fractures
WHY IS WEIGHT-BEARING EXERCISE IMPORTANT?
In weight-bearing exercise, bones and muscles of the legs and trunk work against the force of gravity while they bear the weight of the body. Activities like walking, jogging, step aerobics, dancing and stair climbing are all examples of weight-bearing exercise, as are sports that involve running and jumping such as soccer, basketball, volleyball, racquet sports and others. Weight-bearing exercises are the most effective forms of exercise for maintaining strong bones, especially the bones of the hip and spine. Everyone should participate in weight-bearing exercise, not only to maintain strong bones, but to maintain heart health.
Individuals who are in good general health and are trying to reduce their risk of osteoporosis will be able to do much more vigorous and frequent exercise than those who have more complicated health issues or have a greater risk of fracture. Individuals whose fracture risk is moderate or high may need to participate in lower impact weight-bearing exercises.
Choose exercises that are appropriate for your fitness level, abilities and health status. When in doubt, start low and go slow! Swimming and cycling are not weight-bearing as water buoys or lifts the body and cycling is done in the seated position, which means the legs are not bearing the person’s weight.
WHAT IS STRENGTH TRAINING AND HOW CAN IT HELP PREVENT FRACTURES?
Strength training refers to exercise wherefree weights (dumbbells), weight machines or exercise bands are used to make the bones and muscles work by lifting, pushing or pulling a “load.” Strength training improves muscle mass and strength, and it can increase spine and hip bone density and strengthen bone.
HOW DO I GET RID OF THE HUMP ON MY BACK OR PREVENT ONE FROM DEVELOPING? –
POSTURE TRAINING
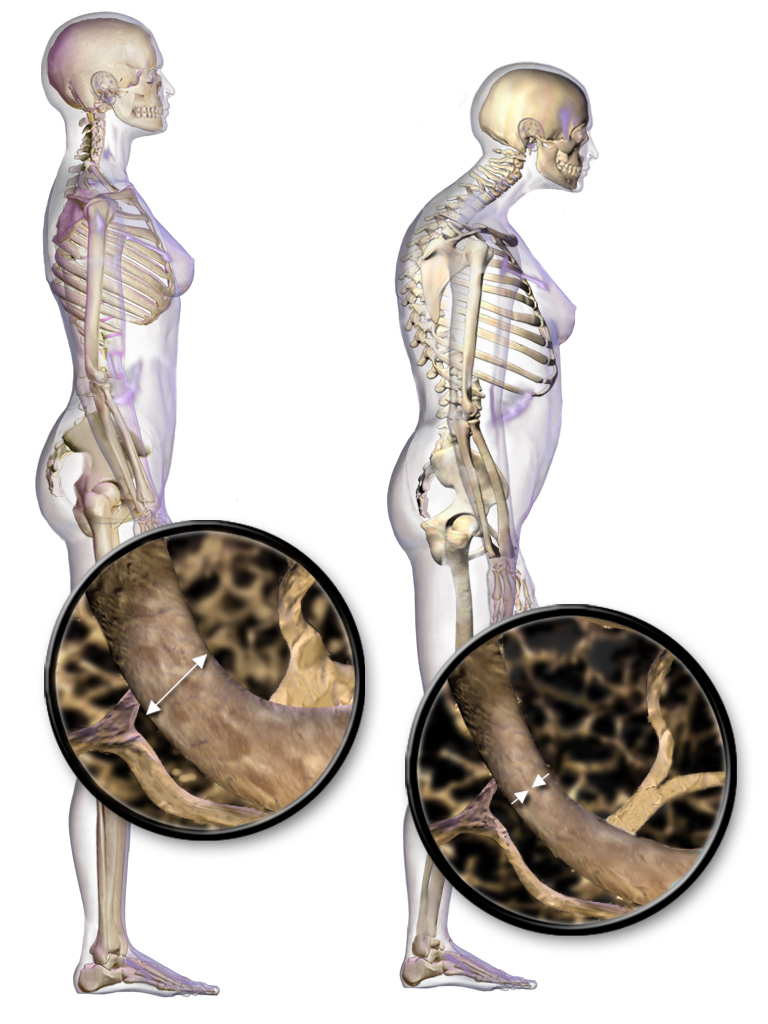
Some kyphosis (a forward curvature of the spine) can be normal, but weak back muscles or spine fractures can produce more rounding of the back called an exaggerated kyphosis. The more an individual bends or slouches forward, the more pressure he or she is putting on the front of the vertebrae, which puts the vertebrae at even greater risk for breaking (fracturing). Posture training exercises emphasize good neck, back and shoulder positioning. Proper alignment of the spine by sitting or standing up straight with the shoulders back can strengthen the back muscles, improve general comfort and help maintain good balance.
HOW DOES EXERCISE HELP TO PREVENT FALLS AND FRACTURES? – BALANCE TRAINING
Exercises that improve balance and coordination can also reduce falls and fractures. Balance exercises help us maintain balance when unexpected or unbalanced movements in daily life occur. However, when balance is challenged, there is an increased risk of falling. For this reason, it is important to observe safety precautions while doing balance training, such as having a table, wall or chair nearby to hold onto, or by having someone “spotting” you. Tai chi is a very safe and effective low impact form of exercise that improves balance and reduces the risk of falls.
WHAT ABOUT STRETCHING – IS IT BENEFICIAL?
As we age, we lose flexibility from inactivity and poor habits, which can contribute to pain and stiffness. Pain and stiffness can result in a vicious cycle. The more pain and stiffness we experience, the less likely we are to exercise, and so we lose bone and muscle strength as a result. This in turn increases the risk for falls and broken bones, which will just add more pain and stiffness. Stretching exercises help to break this vicious cycle by improving flexibility and range of motion.






 What is Osteoporosis?
What is Osteoporosis?